A psychological intake sets the tone for every step that follows in therapy. In your first session with the client, you are not just writing therapy intake notes. You are building trust, identifying risk, and laying out a clear path for comprehensive care.
When the intake appointment goes well, you thoroughly understand the client's concerns and plan effective treatment. But if it goes poorly, you may miss essential information, misdiagnose, or fail to make the patient's life better.
This guide explains the definition of a psychological intake, key elements to include in your form, and tips for conducting the first meeting. You'll also learn the templates and psychological tools you can use to run the session with care and focus.
What is a Psychological Intake?
A psychological intake is your first structured meeting with a new client. This is where you gather important details about the patient.
You ask them about their symptoms, medical history, strengths, support systems, and coping skills used. Through active listening and objective observations, you gain a deep understanding of the client’s situation.
This intake process matters because it shapes your therapeutic relationship with the client.
A clear, respectful intake helps patients feel heard, guides your clinical analysis, and supports focused care from the very beginning.
Key Elements of a Well-Designed Intake Form
Below are the key parts to include in your therapy intake form.
Client Identifying Information
Ask for the client's full name, date of birth, preferred pronouns, address, phone number, email, and other contact details.
You should also include space for an emergency contact person and the name of a primary care doctor if the client has one.
These items matter because mistakes can lead to billing errors, missed follow-ups, or risk gaps. Accurate data also helps you match records across providers when the client signs a release.
Presenting Concerns
Presenting concerns tell you why the client is seeking treatment.
Allow them to explain their main problem in their own words, the onset date, what makes it worse or better, and how it affects daily life. Add space for the client’s treatment goals.
This part guides your focus in the first session and helps you develop a shared treatment plan.
Current Symptoms and Cognitive Functioning
This part is where you gather what the client feels and what you see.
Use clear checklists for mood, worry, trauma signs, anger, sleep, appetite, attention, and memory. Add questions on physical symptoms that may link to stress, such as headaches, stomach pain, or fatigue.
You should also ask about how symptoms impact work, school, relationships, and overall daily life.
When you collect such information, you can quickly identify patterns that may point to risk, substance use, or a need for medical follow-up.
You can also use this data as a baseline for later comparison because symptoms change over time.
Mental Health History
Mental health history provides additional context for the client's current concerns and symptoms.
Ask about previous diagnoses, therapy, hospital stays, crisis visits, and medications taken. Then, follow up on what helped, what did not, and why they stopped therapy if they did.
You should also ask about past self-harm behaviors, suicidal ideation, substance abuse, or harm to others.
This section of the intake form helps you avoid repeating failed treatment plans. It can also show if current issues are new or part of a longer cycle. It even helps you form an early clinical view without rushing to labels.
Medical and Health Background
This part covers health issues that affect the client's mood, thought, and behavior.
Ask about major illnesses, sleep issues, pain, head injury, hormone changes, and other medical conditions tied to mental health, such as thyroid problems.
Then record the client's current medications, doses, and side effects, as well as any supplements the client is currently taking.
Knowing the patient's medical background is important because many mental health signs overlap with body-based causes.
If you capture this data early, you can decide when to consult with a primary care physician, adjust your treatment plan, or move more slowly due to health limits.
Family, Social, and Developmental Context
Explore the client’s background and current living situation. Ask about their childhood, major life events, education, work, housing, and support systems.
Include personal and family history of mental health and substance problems. You should also consider culture, faith, and community ties.
These context clues help you identify triggers and supports beyond reported symptoms. They also help you set treatment goals that fit the client’s real life, not an ideal one.
Coping Skills and Strengths
Do not skip strengths in intake. Ask what the client does to calm down, solve problems, or get support. Include past wins, personal values, hobbies, and people they trust.
This section gives you tools you can build on right away. It also balances the tone of the mental health intake.
Clients often arrive feeling broken or ashamed. When you highlight coping and strengths early, you give them hope and gain their trust.
Insurance and Payment Information
Collect the insurer name, plan type, member ID, and coverage limits.
Ask the patient if they would like to use insurance or pay out of pocket. Add space to accommodate needs for invoices or superbills.
Don't forget to include policies on late cancellations, no-shows, and fees for future sessions, if applicable.
This section matters because money stress can derail care. If clients feel blindsided later, they may stop therapy.
Transparent payment items also reduce administrative burden and help your staff handle claims smoothly.
Informed Consent and Client Acknowledgments
Documented consent protects both you and the client from legal issues that may arise.
Make sure the patient knows what therapy is and how you work. Include the purpose of services, expected benefits, limits, and data retention policies.
State the limits of data privacy, such as danger to self or others, abuse reporting, and court orders.
Ask the client to sign that they understand and agree to all your policies. This builds trust and supports ethical practice.
Psychological Intake Form Example
Here's a psychological intake form template you can use:
Client information
- Name:
- Date of birth:
- Contact details:
- Address:
- Emergency contact (name/relation/phone):
Reason for visit:
Current concerns (check any)
☐ Low mood ☐ Worry ☐ Panic ☐ Trauma stress ☐ Anger/irritability
☐ Sleep trouble ☐ Appetite change ☐ Low energy ☐ Difficulty concentrating
☐ Intrusive thoughts ☐ Avoidance ☐ Compulsions ☐ Hearing/seeing things
Other: __________
Mental health history
- Prior therapy? What helped/didn’t help?
- Past diagnoses or hospital stays?
- Current/past psych medications (name, dose, helpful or not, side effects):
Medical background
- Major health issues or pain:
- Current medications/supplements:
- Alcohol/drug use (type, how often):
Safety and risk assessment
- Thoughts of self-harm? Yes/No
- If yes: plan, intent, access to means?
- Thoughts of harming others? Yes/No
- Feel safe at home? Yes/No
Life context and environmental factors
- Who do you live with?
- Family mental health or substance history:
- Employment status:
- Job satisfaction:
- Military background:
Coping skills and strengths
- How do you typically cope with stress or anxiety?
- Who do you rely on during difficult situations?
Payment
- Insurance company and plan:
- Member ID:
- Self-pay or insurance billing?
Consent
☐ I understand the nature of therapy and its limits.
☐ I understand privacy rules and reporting limits.
☐ I agree to the payment policy.
☐ I consent to treatment.
Client signature: ___________________ Date: __________
Clinician signature: ________________ Date: __________
How to Conduct a Successful Psychological Intake Session
Here are some tips on running your intake session with confidence, focus, and care.
1. Review Intake Forms in Advance
Before the initial appointment starts, read the client’s intake forms. Spend a few minutes scanning for their main concerns, risk factors, and important mental health history.
Mark items you need to follow up on, such as past self-harm, substance abuse, or recent losses. Take note of gaps or unclear answers.
You should also prepare thoughtful intake questions based on information gathered to avoid wasting valuable session time.
If you use screeners or psychosocial assessments, score them early and write down the top results ahead of the session.
2. Greet and Orient the Client
Once you're facing the client, greet them warmly and offer a seat.
Tell them what to expect today. Specify the duration and the key elements you will cover during the therapy session.
Explain that you will ask questions, write notes, and give the client time to share their thoughts.
For example, you can say, "Thanks for coming in today. Before we start, I want you to know this is your space. You can share only what you feel ready to share, at your own pace. I’ll ask some questions to understand what’s been going on and how I can help. If anything feels too hard to talk about right now, you can tell me, and we can slow down or skip it for today. My goal is to understand you and support you."
This is the first step of building a safe environment and forming a therapeutic alliance with the client.
3. Clarify Presenting Concerns and Symptoms
After the client is comfortable, ask them about their primary concerns. What had led them to seek help now?
Summarize what you've read on the therapy intake form and confirm that you got it right.
Be clear about onset, length, and how often symptoms show up.
You should also review significant changes that may trigger symptoms, such as a new loss, health condition, job stress, or family conflict. Use simple follow-up questions like “When did this start?” or “What happens right before it gets worse?”
4. Discuss Mental Health Concerns
Shift from the main concern to a thorough discussion of the client's well-being. Ask about mood, worry, panic, trauma stress, anger, obsessions, compulsions, and any unusual thoughts or perceptions.
You should also check sleep, appetite, energy, and focus. Then, let them describe what a “hard day” looks like and what a “good day” looks like.
Summarize patterns you notice and link them to the client's self-reported symptoms.
This process involves active listening, careful follow-ups, and steady pacing. It's important to write down your objective observations and avoid labels until you're certain.

5. Ask About Therapeutic Goals
After you understand the concerns, ask what the client wants from psychiatric care. Use questions like, “What would feel better in a few months?” or “If therapy works, what changes first?”
Let them describe goals for the therapy. Then, work with them to translate big wishes into small targets.
You can also explain possible treatment options in general terms and how they connect to your therapeutic approach.
If relevant, ask about previous goals in therapy and what felt useful. Share how these objectives guide your plan and lead to better outcomes.
6. Conduct a Mental Status Exam
A mental status examination (MSE) is a structured intake assessment that evaluates a user's appearance, behavior, cognitive health, mood, speech, and thought process.
This initial assessment provides a detailed picture of the client's current mental functioning during the session, not just what they report on paper.
To conduct an effective mental status exam, observe the client's appearance and movements. Listen to speech clarity, tone, and volume.
Ask how they feel, and watch if their emotion fits the story. Pay close attention to how thoughts flow and whether they make sense.
You should also test their attention and memory with simple questions. For example, you can ask, "What did you do earlier today before coming here?"
7. Screen for Risk Factors and Safety Issues
Screen for safety early and with a calm tone. Normalize the questions so the client does not feel judged or defensive.
Ask directly about suicidal ideation, past self-harm, and any current intent or plan. Check access to means and past attempts.
You should also review the client’s history of drug abuse and current use of alcohol or recreational drugs. Link usage to mood, sleep, and risk. If risk is present, slow down and focus on safety.
Develop a simple safety plan with clear steps and crisis contacts before the session ends.
8. Evaluate Strengths and Support Systems
Do not focus only on problems. Ask what helps the client cope and who stands with them. Explore close family members, friends, partners, work ties, faith groups, and community links.
For example, if the client has healthy family dynamics, mention the value that their relatives may bring outside the therapy session.
Then, find out who else is on their care team. For example, they may work with a primary physician or a psychiatric nurse practitioner. Explain how those providers can offer additional support if risk rises or medication management is part of the plan.
End the session on a positive note by naming at least one strength you heard.
9. Formulate Initial Clinical Impressions
Once the intake session has ended, you can formulate your initial impressions. Consider the facts that you've learned during the session and the results of the biopsychosocial assessment the client has completed.
Compare their written answers with what you observed and heard live. Look for themes across symptoms, health, relationships, work, and stress.
Note what seems most likely, what is still unclear, and what you need to rule out later. Keep your view flexible.
Share this summary with the client and ask if it fits their experience. This is an important step because it guides future sessions, your treatment plans, and your referrals.
10. Plan Next Steps
End the psychological intake process with a clear path forward.
First, restate the client's main concerns and what you think is driving them.
Then, match the next steps to what you learned. If the client is a good fit, determine future session focus and how often you suggest meeting.
If you need more data, tell them what you will assess next, like a few mental health screeners or a follow-up visit. This helps you develop customized treatment plans that align with the client's actual mental health concerns.
Think a referral is better? Explain why, offer options, and write a referral letter.
Useful Tools for the Psychological Intake Process
Consider using the following tools to support your psychological intake process.
Structured Diagnostic Interviews
These are guided question sets that help you cover key symptoms in a consistent order. They reduce missed areas and support clear first impressions.
Popular examples include the Structured Clinical Interview for DSM-5 (SCID-5), Mini International Neuropsychiatric Interview (MINI), and Diagnostic Interview Schedule (DIS).
Psychological Assessments
These refer to brief measures or longer tests you use before, during, or after the mental health intake. They give a clear baseline on the client's symptoms, stress, function, and change over time.
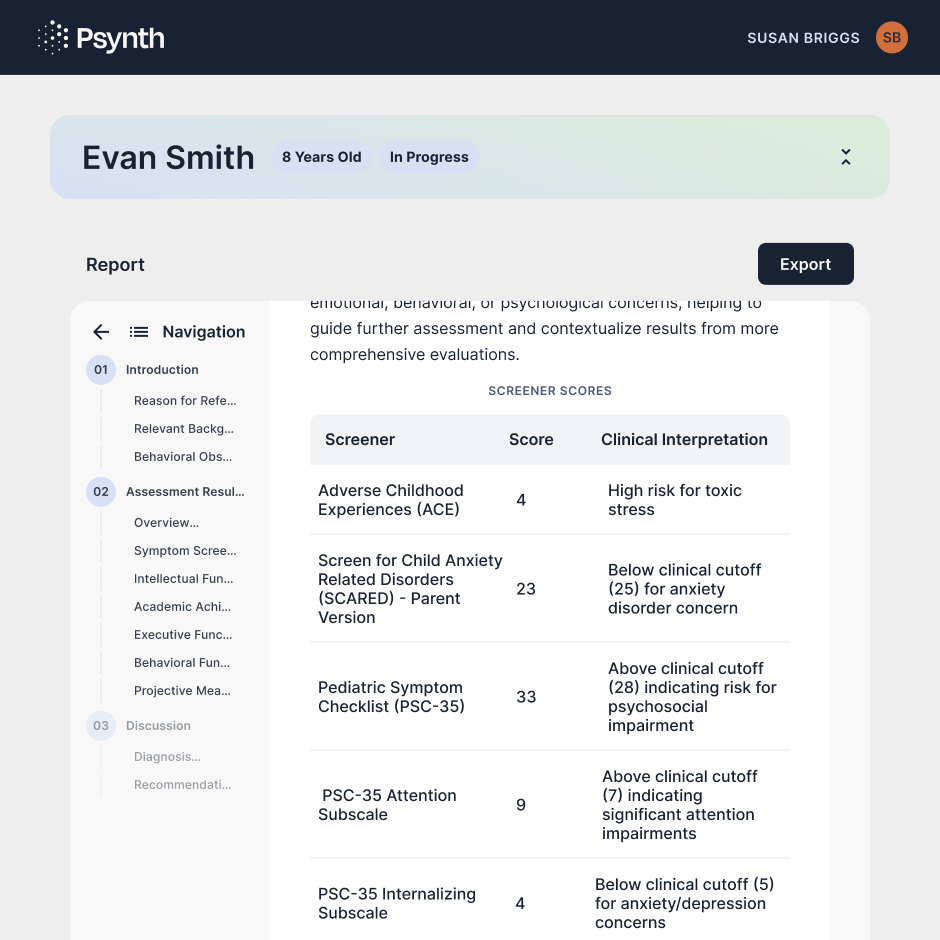
You can pick broad screeners for mood, worry, trauma stress, attention, sleep, or substance use. Then, add focused tools based on what the client reports. Doing so helps you confirm patterns, track progress, and guide early goals.
AI-Assisted Reporting Software
This specialized software for psychologists turns your intake notes, test results, and clinical observations into draft reports. It can help you organize the client's history, symptoms, mental status findings, and a working diagnosis in a clear format.
However, you still control what goes in, what comes out, and what becomes final. Always read the draft, correct mistakes, and adjust the tone to fit your clinical voice.
Use AI-assisted reporting tools to save time on structure, not on thinking.
Ambient Listening Technology
Ambient listening software is a type of mental health technology tool that records the session audio and turns it into a draft note or summary.
It reduces typing during intake, allowing you to remain focused on the client’s words, tone, and emotion.
Make sure to ask for clear consent to maintain compliance. Explain what the software does with the data, and let the client opt out anytime.
After the session, review the automatically generated draft for errors, missing context, or wording that feels off. You still have the final say and should not let the software replace your work as a psychologist.
Psynth Transforms Psychological Intake Forms and Notes Into High-Quality Reports

Psynth transforms psychological intake notes, test results, and clinical observations into professional reports in minutes, not hours.
The AI software is built on validated best practices in psychological reporting and input from expert psychologists. This ensures high-quality, PhD-smart drafts ready for your review and finalization.
Psynth also lets you customize reports to match your voice, preferences, and clinical needs. It even runs automated quality checks to guarantee data accuracy.

Psynth isn't designed to replace your work. It simply handles the time-consuming parts of report writing, so you can focus on client care and clinical analysis.
In fact, adopting Psynth has cut reporting time in half for Coast Psychology. As Dr. Morizio puts it, "I spend far less time on tedious tasks like formatting and score transcription, and more time on clinical synthesis."
Try Psynth for free today to complete reports in minutes!
FAQs About Psychological Intake
What is psychological intake?
Psychological intake is your first session with a new client. This process involves gathering key facts about why they came in, what symptoms they have, how life is going, and what risks may be present. It also covers previous medical history, environmental factors, and treatment goals. A successful intake session provides a clear starting point for care.
What is a psych intake like?
A psych intake feels like a guided conversation. You welcome the client, explain what will happen, and ask focused questions. You listen to their story, ask follow-ups, and write down notes. To confirm clinical impressions, you may use screeners or conduct assessments. You end the intake by summarizing what you've learned and sharing next steps.
What are some examples of intake?
Examples include a standard adult intake for mood or worry, a child intake with caregiver input, and a couples intake focused on the relationship. Each one matches the referral need.
How long does a psychological intake take?
Most psychological intakes last 50 to 90 minutes, depending on the setting and client needs. Private practice often uses one full session. Hospitals or clinics may split intake into two visits. More time may be needed if the risk is high or the client's mental health history is complex.



