Mental health documentation is part of your daily work as a psychologist. You write it to document care, track the client's progress, and show the reasons behind your clinical interpretations.
However, this documentation involves more than therapy session notes. It also refers to assessment reports, diagnostic summaries, treatment plans, case formulation statements, and safety or crisis plans.
With so many document types, it is easy to feel confused about what to write and how much detail to add.
This article shows clear examples of mental health documentation used by psychologists. You'll also learn about the mistakes to avoid and the ethical considerations when documenting clinical work.
What Is Mental Health Documentation?
Mental health documentation is the written record of the care you provide. It captures what you learn from the client interaction, what you do, and how your patient responds over time.
For psychologists, clinical documentation includes more than session notes. It can also be intake records, assessment reports, diagnostic write-ups, treatment plans, case formulation statements, safety plans, and discharge notes.
Proper documentation matters because it supports your clinical thinking and helps you track progress from one visit to the next.
Complete notes and records also support billing, legal needs, and teamwork with other mental health professionals. They even help you identify patterns, plan treatment interventions, and provide better patient care.
Common Examples of Mental Health Documentation Used by Psychologists
Psychologists use many document types to support client care. Here are the ones you will use most often in your clinical practice:
Therapy Intake Notes
Therapy intake notes record what you learn at the start of care. You write them during or right after the first session.
This type of mental health documentation explains why the client seeks therapy, what symptoms they report, and how those symptoms affect daily life.
Good intake notes also list key issues, such as risk factors, medical history, past therapy, previous suicide attempts, and harmful coping strategies.
Many psychologists use structured intake forms, while others write a short narrative summary. Common types of intake notes include cognitive behavioral therapy (CBT) intake, child intake with caregiver input, couples or family intake, and trauma-based intake.
Mental Health Progress Notes
Progress notes are your record of each visit. You write them after every therapy session to capture key details of what you saw, what the client shared, and what comes next.
You can use structured templates to write progress notes.
SOAP notes are the most popular and follow the SOAP format: subjective, objective, assessment, and plan. They examine both subjective and objective data, then include your interpretation and the next steps based on the information gathered.
If you want something shorter, DAP progress notes work well by focusing on data, your assessment, and your plan.
BIRP (behavior, intervention, response, plan) notes are also common, especially if you want to document the client's behavior or cognitive interventions.
Regardless of the template used, mental health progress notes should link your objective observations to what you did next. They're also a useful clinical tool for tracking the client’s progress throughout the treatment journey.
Psychotherapy Notes
Psychotherapy or process notes refer to a psychologist's private notes that are not meant to be shared with others. They typically include the therapist’s observations of mood shifts, meaning, or defenses of the client.
Psychologists write psychotherapy notes for multiple purposes. They use these notes to plan next sessions, reflect on what is happening in the therapy relationship, and report details that do not belong in the client's official medical record.
Psychotherapy notes do not follow a standardized format. They can be written in free style without including critical details, such as diagnosis and treatment plans.
Psychological Assessment Reports
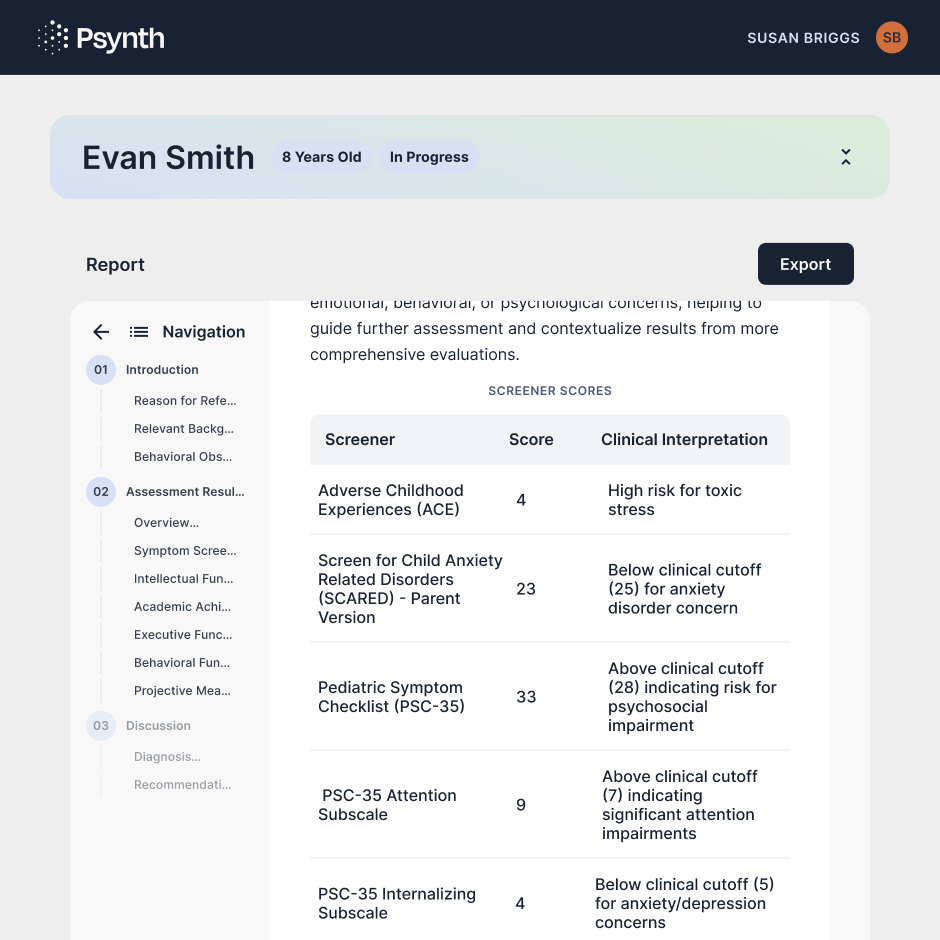
Psychological assessment reports summarize what you learn from testing and evaluation.
You write them to answer a clear referral question, guide diagnosis, and shape treatment.
You may draw from structured interviews, standardized tests, rating scales, and risk assessment tools. You can also use functional tools that show how symptoms affect work, school, sleep, or relationships with family members.
Many psychosocial assessment reports include the presenting problem, environmental factors, risk factors, significant life events, and diagnosis based on test results and other essential details captured.
For example, if test results point to major depressive disorder, explain how other data lines up with symptoms and impact.
If you see avoidance behaviors, describe when they show up and how they shape the client's daily life.
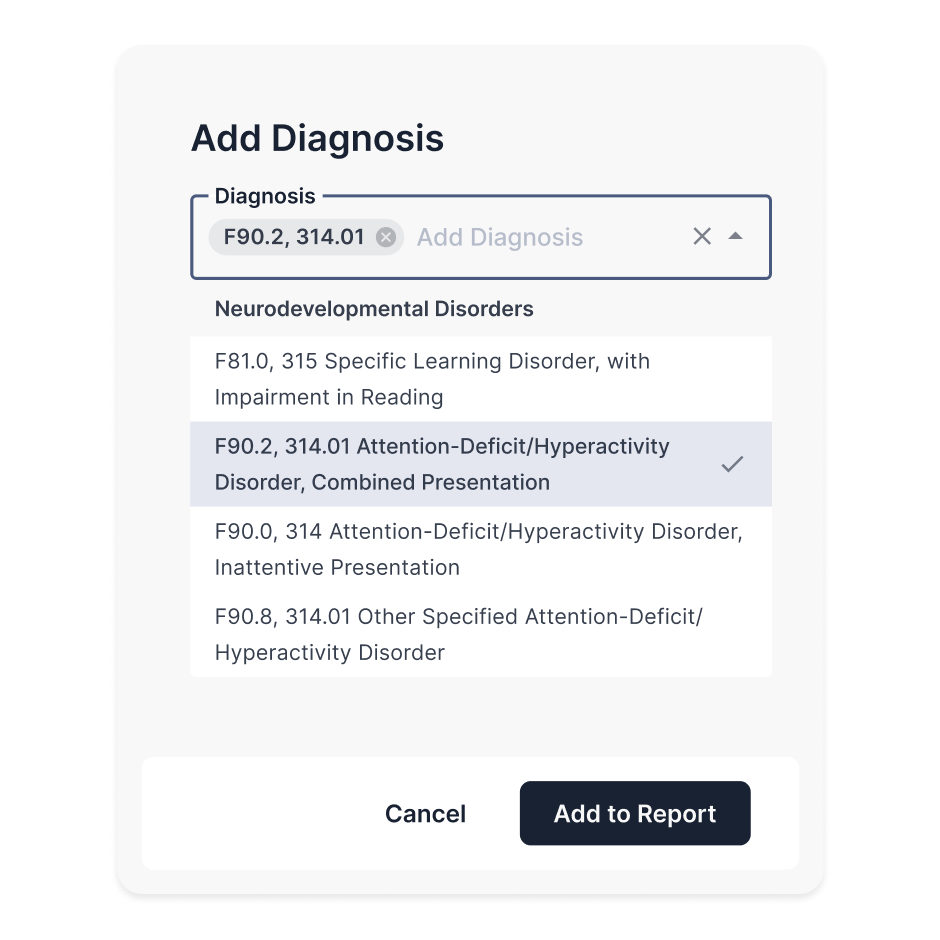
Diagnostic Reports
Diagnostic reports focus on stating and supporting a mental health diagnosis. These reports combine key findings in a structured way.
When writing diagnostic reports, the first thing to include is the reason for referral or the client's self-report of current symptoms.
Next, you provide relevant information, such as medical history, current stressors, and previous treatment. Add brief behavioral observations from sessions and testing.
Then, summarize assessment results, including interviews, rating scales, and any test data. After that, state the diagnosis and explain why it fits the full picture.
For example, if the client reported depressive symptoms, ask them how often these symptoms occur, how severe they are, and how they affect daily life. You can then conduct relevant assessments to confirm or reject the patient's explanation of their mental health problem.
End with clear recommendations tied to the diagnosis, such as therapy focus, follow-ups, or referrals for medication evaluation. Keep the tone factual and easy to review.
Treatment Plans
Treatment plans lay out what you and the client will work on and how you will do it. They keep therapy focused and provide a clear record of the methods used to treat mental health conditions.
You write these plans early in care and update them as things change.
Make sure to list the main problems, long-term goals, short-term objectives, and the steps you will use in sessions. You should also note how often you will meet and how you will check the client's progress.
Common examples of treatment include CBT techniques or mindfulness exercises for mood and worry, trauma plans with pacing and safety steps, and skills-based plans for emotion control.
You may also introduce cognitive restructuring techniques to challenge thought errors.
If the client exhibits signs of anxiety symptoms, you can teach breathing exercises and other relaxation techniques.
Keep treatment goals specific and tied to daily life, so you can observe the client's response and measure progress over time.
Case Formulation Statements
Case formulation statements explain how you understand the client’s struggles. They connect the client’s history, current triggers, thoughts, feelings, and behaviors into one clear story.
You write them to guide treatment choices and to keep your work grounded in a shared view of the problem.
A good case formulation has several essential elements. Start with the main concerns and symptoms. Add the factors that may have led to them, like early experiences, losses, trauma, or family patterns.
Next, document what keeps the problem going now, such as beliefs, coping habits, or social stress. Mention the client's strengths and support systems that can help change happen.
Then, state your working theory of how these pieces fit together. End with what this means for care, such as which goals matter most and which methods fit best.
Keep it simple, specific, and easy to update as you learn more about the client's unique situation.
Crisis and Safety Plans
Crisis and safety plans are written steps for what to do when a client is at risk of harm. They are especially important when warning signs show up or when a client has a history of harm to self or others.
A structured plan gives a clear path to follow during high-risk moments, both for you and the client.
These plans often start with a short risk summary. For example, you may note that the client presented suicidal thoughts and describe the level of risk in plain terms.
Next, list early warning signs that the client can spot.
For the actual plan in case of harm, add coping skills they can try first, such as grounding or calling a support person. Include people and places that help them feel safe.
Write down emergency contacts, local hotlines, and when to go to urgent care or the ER. Close with follow-up steps and how often you will check in.
Correspondence and Referral Letters
Correspondence and referral letters are written updates you share with other healthcare providers to ensure continuity of care.
You use them to pass along needed context, request additional services, or explain why a referral fits the client’s needs. You may write to psychiatrists, primary care doctors, school teams, social workers, and other mental health professionals.
To write an effective correspondence or referral letter, you should briefly explain why you are writing to the reader.
Provide a summary of the client’s main concerns and what you have seen so far. Mention key points from previous sessions, but keep it factual.
State any current diagnosis and risk level if it matters for next steps. Then, list what you recommend and why.
End the letter with your contact information and a note that you are open to follow-up.
Avoid personal opinions and stick to only what the next provider needs to know.
Discharge or Termination Documentation
Discharge or termination documentation is the final record when therapy ends. You write it to conclude care clearly and safely. It may be planned, like when goals are met, or unplanned, like when a client stops coming.
A discharge note usually includes why care ended, the main issues you worked on, and the progress made. List the methods you used and how the client responded.
Document the skills the patient earned that support ongoing mental stability. Add a risk check at the end, even if the risk is low.
Then, write your aftercare plan, such as referrals, support groups, homework assignments, or follow-up sessions. You may share this note with the client and with other providers if you have the patient's consent.
Consider using customizable templates when writing termination letters to maintain consistency while still fitting each case.

Mistakes Psychologists Should Avoid in Mental Health Documentation
Even skilled psychologists can make mistakes when documenting care. Here are the common mistakes to avoid to ensure accurate documentation:
Including Excessive Details
Writing too much can hide what matters most and can expose private facts that do not support care.
Focus on the client’s main concerns, your clinical work, and next steps. Leave out side stories, full histories, or extra quotes unless they shape treatment.
The goal is to balance detail and brevity so the readers can quickly understand the note and grasp the case.
Using Vague, Subjective Language
Vague wording makes notes hard to trust. Phrases like “doing better” or “seems off” do not show what you saw or how you decided.
Instead, describe what you observed in plain, behavior-based terms. Provide short examples when needed.
Tie your clinical view to the client’s report, your observations, and any measures you used. This keeps your note clear, fair, and easy to defend if reviewed.
Overusing Clinical Jargon
Heavy jargon can confuse readers and weaken care links. It may also sound cold to clients who read their records.
Use clear and simple terms as much as possible. Add clinical terms only when they help with diagnosis or treatment plans. If you need to use a term, explain its meaning to avoid confusion.
Copying and Pasting Old Therapy Notes
Copy-paste habits can create errors.
Old notes, even if they're documented in the past week, may no longer fit the current session, the client’s mood, or the plan. They also tend to repeat facts that are no longer applicable.
If you reuse a structure, always rewrite the content. Check dates, symptoms, risk level, and goals.
Writing updated notes shows real care and protects your business if the record is reviewed later.
Delaying Documentation Until Details Are Forgotten
Waiting too long leads to documentation gaps and weak notes. Memory fades fast after several sessions. Small facts like shifts in tone, new stressors, or rapid speech may be lost by the end of the day.
Write notes as soon as you can while the session is clear in your mind.
Consider using mental health technology tools, such as ambient listening software, to transcribe conversations in real time. This lets you stay present during the session instead of worrying about note-taking.
Neglecting Risk Assessments and Safety Planning
Do not skip risk screenings, even when a client seems stable. Missing risk assessments creates legal and clinical risk.
Record any thoughts of harm, intent, past history, and protective factors. If a risk is present, develop a safety plan and include follow-up steps.
Failing to Connect Interventions to Treatment Goals
Many psychologists record what they did in session, but do not show how it ties to the treatment plan. When that link is missing, the note reads like a list of actions with no clear goal.
To fix this, name the goal first, then write the intervention as a step toward that goal. Add a brief reason why it currently fits the client’s needs.
Then, end with the patient’s response and the next steps. This shows a clear line from problem to action to outcome, which keeps care focused over time.
Legal and Ethical Standards in Mental Health Documentation
Clinical records and documentation should protect clients, support care, and meet the rules that govern your work. Below are the legal and ethical considerations to keep in mind:
HIPAA Compliance
The Health Insurance Portability and Accountability Act (HIPAA) sets the baseline for data privacy and security in the healthcare industry.
To meet HIPAA compliance standards, your notes should include only what is needed for care, billing, and safety. Use clear, factual language and avoid personal content.
You should also store records in secure systems with access controls, encryption, and strong passwords.
Software for psychology is becoming a crucial tool for any clinician. If you use such digital platforms to write mental health documentation, make sure they are HIPAA-compliant.
Informed Consent
Informed consent is an ongoing process you must record. Document that you explained therapy goals, risks, limits of privacy, fees, and the client’s rights.
Then, take note of the client's consent for telehealth, testing, recording, and coordination with other providers.
Make sure to ask for their updated consent when care changes, such as adding a new method or shifting to a new setting.
Zero Data Retention Requirements
If you use digital tools to support your clinical work, pay close attention to their data retention policies.
Some platforms promise zero data retention, meaning they do not store client content after use. This can lower privacy risk, but only if the claim is real and in writing.
Always review vendor policies, storage terms, and security features before using the software. Do not enter more client data than needed.
Client's Rights to Access or Amend Clinical Records
Clients can request access to their records in most settings. They may also ask for changes if they think something is wrong.
You should know your state rules and document how you respond. For example, if you granted access, document what you shared and when. If you deny part of a request, state the legal reason and your clinical view.
Keep your tone respectful and factual. Proper documentation protects the client’s rights and supports your professional duty.
Subpoenas, Court Orders, and Documentation Readiness
Your records may be requested by courts, employers, or other agencies. A subpoena is not always the same as a court order, so review each request and follow your legal process.
If needed, consult your legal counsel or your licensing board. Document what you received, how you verified it, what you released, and what you withheld.
Psynth Turns Mental Health Documents Into Accurate, High-Quality Reports

Psynth uses AI to process different mental health documentation types and automatically transform them into high-quality diagnostic reports. This means you can review and finalize psychological reports in minutes, not hours.
Each draft is customizable using AI-assisted prompts or manual input. It also includes clear descriptions and data visualizations designed to improve patient understanding.
Psynth supports smarter diagnoses by providing evidence-based findings and clear explanations. These help you understand the full picture, so you can focus on nuanced analysis.
For data security, the platform meets HIPAA compliance requirements through encryption and a signed business associate agreement (BAA). It guarantees the secure processing, storage, and transmission of sensitive health information. Data is never used, sold, or repurposed in large language models.
Psynth isn't designed to replace psychologists and remove the need for assessment. It simply helps you write reports faster and with less effort, leaving you free to focus on your patients.
Try Psynth for free today to reclaim valuable time spent on mental health documentation!
FAQs About Mental Health Documentation Examples
What is an example of a mental health status note?
A mental health status note is a short, focused summary of how the client is currently doing. For example: “Mood low, flat affect, thought process clear, no delusions, denies self-harm, poor sleep, fair insight.” You often include this documentation in progress notes to support your clinical view.
What are the five C's of mental health?
The five C’s are a simple way to group key parts of mental health: connection, coping, calm, confidence, and control. They remind you to look at how a client relates to others, handles stress, remains steady, trusts themselves, and manages their emotions or behavior.
How to document mental health status?
Start with what the client reports, then add what you observe. Break them down into clear areas, such as mood, affect, speech, thought process, perception, insight, judgment, and risk. Keep language factual.
What are the five P's of mental health assessment?
The five P’s help you organize a full case view: presenting problem, predisposing factors, precipitating factors, perpetuating factors, and protective factors. They help you identify what's happening, why it may have started, what triggered it, what keeps it going, and what supports recovery.



