For many psychologists, note-taking is among the least enjoyable parts of the workday. This task often requires a lot of effort and time, which you'd rather spend on patient care.
However, despite being an administrative burden, writing notes is a key part of your clinical, legal, and compliance duties. Accurate notes protect you professionally, support continuity of care, and track the client’s progress over time.
This guide will help you write effective notes. You’ll learn the key types of psychologist notes, popular templates to ensure consistent writing, and digital tools you can use to save time without losing accuracy.
What Are Psychologist Notes?
Psychologist notes, as their name suggests, refer to written records created by psychologists after client sessions.
These notes capture key details about the client’s behavior, condition, and progress. They serve as a professional record of the psychologist’s observations and clinical reasoning.
Psychologist notes help mental health professionals track progress over time and guide future treatment plans. They also provide a legal and ethical record of care.
Well-written notes help ensure continuity between sessions and support collaboration with other providers when needed.
Different Types of Psychologist Notes
Not all psychologist notes serve the same purpose. Each type records different kinds of patient information. Here are the two main types you can encounter:
Psychotherapy or Process Notes
Psychotherapy notes, often called process notes, are your private notes written for personal use. These notes capture your thoughts, feelings, and reflections about a session.
You might include insights into treatment direction, potential diagnoses, or other observations that don’t belong in the client’s official record.
Unlike progress notes, psychotherapy notes are not meant to be shared with clients, insurance companies, or other mental health professionals.
They’re protected under privacy laws and stored separately from the client's medical record.
Progress Notes
Progress notes refer to mental health documentation that records what occurred during therapy. It includes important details about the session, such as the client's response to questions, observable behaviors, moods, symptoms, and the intervention techniques used.
Therapy progress notes track the client's condition and treatment status. They help coordinate session details between professionals and document progress over time.
These are also part of the client’s file and may be shared with insurance providers, auditors, or other mental health clinicians. They fulfill legal and ethical standards for clinical documentation.
Popular Templates Used in Psychologist Notes
Using a standardized format helps you write clearly and consistently. The following therapy note templates provide a structured way to capture key session details:
SOAP
The SOAP method is one of the most widely used formats among psychological practices and other healthcare settings. It stands for:
- S (Subjective): The client's subjective experiences, including symptoms, feelings, concerns, and reasons for seeking therapy.
- O (Objective): The psychologist's objective observations during the session, including the client's emotional state, behaviors, tone, and body language.
- A (Assessment): The psychologist's interpretation or clinical impression based on the information gathered.
- P (Plan): The next steps to take, including interventions, future sessions, or follow-up actions.
For example, the client reported feeling overwhelmed and anxious about work (subjective). As a psychologist, you observe restlessness and tense posture (objective). You assess mild work-related anxiety (assessment) and plan to introduce relaxation techniques in the next session (plan).
SOAP notes organize both the client’s input and the therapist’s observations in a logical way. These provide a reliable structure for insurance documentation and supervision reviews.
DAP
The DAP template offers another way to write psychologist notes with a stronger focus on clinical assessment and planning. Here's a quick breakdown:
- D (Data): This refers to critical details gathered from the session, including what was said, done, or observed.
- A (Assessment): The psychologist's clinical judgment and understanding of the client’s current state.
- P (Plan): It describes your next treatment approach, such as therapy techniques, referrals, or follow-ups.
For instance, the patient reported feeling low energy and loss of interest in daily activities (data). You assessed mild depressive symptoms (assessment) and planned to start behavioral activation exercises in the next session (plan).
The DAP format is simple, flexible, and easy to complete after each session. It works especially well for psychologists who want concise notes without skipping important details.
BIRP
BIRP is useful for documenting behavioral or cognitive interventions. It includes the following:
- B (Behavior): The client’s actions, words, and observable mood during the session.
- I (Intervention): The techniques or interventions used by the psychologist.
- R (Response): The patient’s reaction to the treatment approach.
- P (Plan): The outline for upcoming sessions or continued care based on the patient’s response.
For example, the client trembled and avoided eye contact when discussing flying (behavior). As a psychologist, you used cognitive restructuring to challenge their catastrophic thoughts about plane crashes (intervention). Since the patient showed reduced anxiety by the end of the session (response), you planned to introduce guided imagery exercises to prepare for gradual exposure (plan).
Many psychologists use BIRP when writing case reviews because it highlights client progress and clinical outcomes clearly.
How to Write Effective Psychologist Notes
Here are eight simple steps you can follow to write effective therapy notes.
1. Define the Purpose of Each Note
Before writing, decide what kind of note you need to create. This helps you stay focused and keeps your clinical documentation accurate.
Knowing the purpose before you start also helps you include the right information and avoid writing unnecessary details.
For example, when writing progress notes, you should stick to observable facts and measurable outcomes.
For process notes, use them to reflect on treatment direction or patterns you notice over time.
2. Gather Basic Information
Collect essential details for your notes, such as the client’s name or ID number, the psychologist's credentials, the date, and the session type.
You should also include who was present, such as the client alone or with a family member. Then, add the session length and location if relevant, like in-office or telehealth.
Whether you’re writing a progress note, process note, or assessment summary, always verify this information before adding clinical content. Missing these details can cause confusion later, especially when reviewing multiple sessions.
Keeping a consistent header section also helps when sharing notes with insurers or other healthcare professionals.
This step might seem simple, but it’s one of the most important habits for reliable documentation. When the basics are accurate, you save time and reduce mistakes during compliance audits, billing, or treatment reviews.
3. Follow a Structured Format
Choose a documentation style that keeps your therapy notes clear and consistent. Formats like SOAP, DAP, or BIRP help you organize your thoughts and focus on what matters most.
These templates also record information in a logical order, from the client's chief complaint to your plan for the next session.
A clear structure can even improve communication with other professionals who may read your notes. It helps them understand your reasoning and the client’s progress at a glance.
4. Document Observations Objectively
Write only what you see, hear, and measure during sessions, and nothing more. Avoid adding emotion or judgment to your notes.
For example, write “client appeared anxious” instead of “the client was struggling emotionally.” Or, say “client appeared fatigued with dark circles under their eyes” rather than “the client seemed unmotivated.” These phrases describe visible signs instead of assumptions.
Keep your writing tone neutral and factual. Do not include your personal interpretation in this section. Save that for your assessment or process notes if needed for further exploration. The goal is to document behavior, speech, or body language as you observed it.
Objective writing helps you stay professional and protects you during audits or reviews. It's also easier to read, more accurate, and less likely to be misunderstood by other mental health professionals documenting the client’s conditions.
5. Record the Interventions Used
Take note of the specific therapeutic techniques or tools used in the session.
Be specific. Mention if you used CBT (cognitive behavioral therapy) to challenge negative thoughts, guided relaxation to reduce anxiety, or role-play exercises to practice new behaviors.
If you taught coping skills, describe which ones, like deep breathing or grounding exercises. When working with clients in crisis, note if you created or updated a safety plan.
This section shows how you guided the session and why you chose each method. It also helps other professionals understand your clinical reasoning if they review your notes.
6. Summarize the Client’s Progress
Use this section to show how the client is changing over time. Highlight progress, setbacks, and any shifts in thinking or behavior. Focus on facts, not impressions.
Include measurable examples when possible. For instance, note if the client now uses coping strategies more consistently or if anxiety levels have decreased. You can also mention improvements in daily activities or relationships to reflect a better functional status.
Keep your summary brief but informative. Clear record keeping helps you and others quickly see whether the treatment plan is working. It also supports continuity of care when multiple providers are involved.
7. Plan the Next Steps in Treatment
End each therapy note by writing what comes next. Outline specific actions for both you and the client. Include homework, upcoming session goals, or any updates to the treatment plan.
If you adjusted the client’s diagnosis, explain why. Note any changes in symptoms, functioning, or new clinical findings that support your decision.
When safety is a concern, document your risk assessment and what steps you’ll take to manage it.
Keep the plan realistic and measurable. A clear strategy keeps treatment structured, supports accountability, and shows continuity of care in your documentation.
8. Review and Edit Notes for Clarity
Before finalizing your note, take a few minutes to review it carefully. Check that every section is complete, clear, and free from subjective language.
Make sure all observations, interventions, and outcomes are documented accurately. Look for missing dates, session numbers, or details that could cause confusion later.
If you have self-doubt about what you wrote, use that as a sign to clarify or simplify your language.
Lastly, as you review your notes, you should also reassess progress from a broader view. Ask yourself if the document clearly shows where the client stands and what comes next. This saves time during audits and helps maintain professional credibility.
Top Tools for Writing Psychologist Notes and Reports
Using digital tools for writing notes and reports can significantly speed up your work and make it more accurate. Here are the best platforms to consider:
Psynth

Psynth is an AI-powered software that helps psychologists write reports faster and with greater accuracy.
It turns clinical observations, assessment results, and intake notes into high-quality drafts within minutes. This tool reduces the time spent on administrative work so you can focus on clinical analysis and patient care.
The platform supports more than 370 psychological assessments and accepts different file types, including PDFs and handwritten notes.
After uploading your data, Psynth analyzes the information and creates a structured report based on validated, up-to-date best practices and expert input. Each draft includes evidence-based findings, clear descriptions, and data visualizations that are ready for your review.
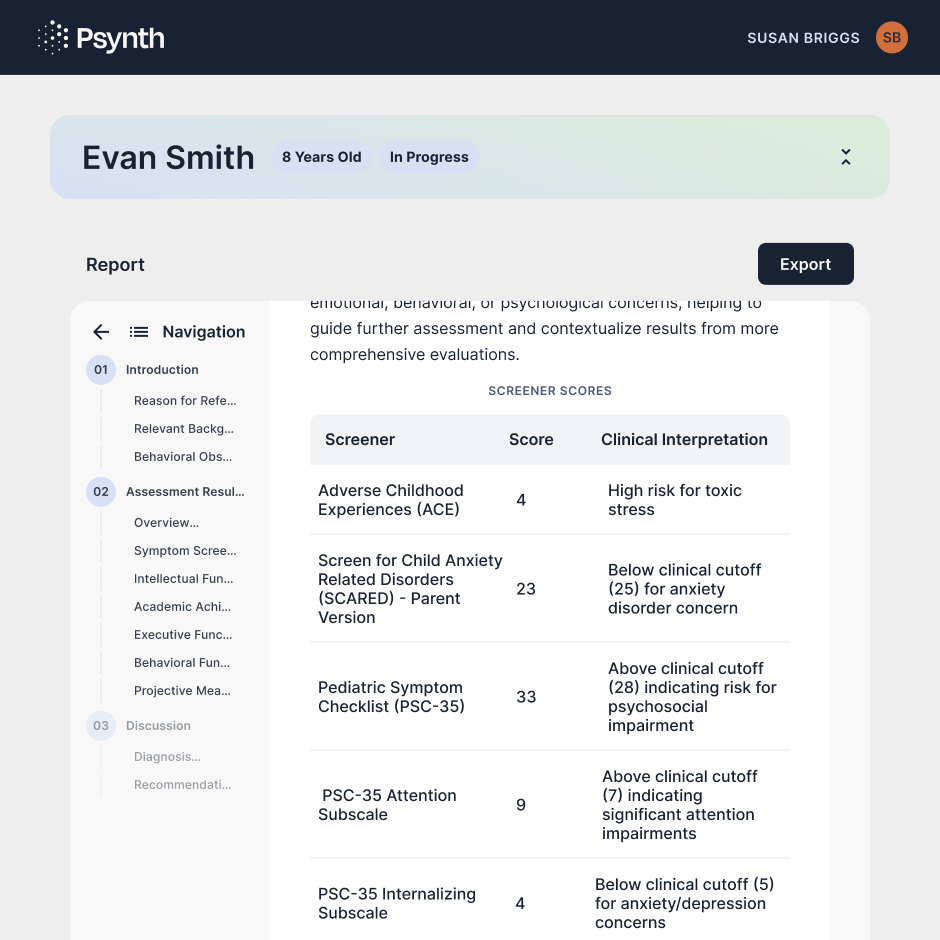
Need to tailor the report to your specific clinical voice or needs? It's also easy to edit any section using your own words or AI-assisted prompts.
You can even run automated quality control checks to ensure data accuracy. Once satisfied with the report, you can export it to Word (.docx) for quick sharing.
With Psynth, every AI-powered report is private and secure. The platform is fully HIPAA compliant with zero-retention language models. Data is encrypted using AWS services that exceed HIPAA security requirements. No information is stored or used for training large language models (LLMs).

Plus, Psynth offers a signed Business Associate Agreement (BAA) with your psychology practice. It protects both personally identifiable information (PII) and protected health information (PHI), consistent with federal law requirements.
If you're seeking software to handle all the work for you, Psynth isn't that. The software is not designed to replace the assessment process. Instead, it simply manages the time-consuming parts of report writing so you can think deeply, diagnose clearly, and reconnect with patients.
Try Psynth for free today to complete reports in less than 45 minutes!
TherapyNotes

TherapyNotes uses an integrated AI solution, TherapyFuel, to help psychologists complete clinical documentation faster.
It listens to your therapy sessions and documents progress notes in real time. Alternatively, you can dictate your findings, and the platform summarizes your notes within seconds.
TherapyNotes also provides access to form-based note templates for various use cases. These include treatment plans, progress notes, and psychological evaluations, among others.
Each template has dropdown menus, checkboxes, and text fields built for quick note-taking. It also pulls client history into new notes, which eliminates redundant typing and saves valuable time.
Meanwhile, a built-in mental health spellchecker reduces spelling mistakes or typos to ensure accurate clinical notes.
For data security, TherapyNotes is private and HIPAA compliant by design. Everything stays within the system, meaning your data is never sold or used to train AI models.
Mentalyc
Mentalyc is an AI-powered documentation tool built specifically for psychologists and mental health professionals.
It offers multiple ways to capture session data: by live listening, uploading a file recording, dictating your summary, or typing notes manually.
After data input, Mentalyc generates a draft in your preferred format (SOAP, DAP, BIRP, etc.). You retain full control over the notes. Make quick edits, customize the layout, or drill down to specific moments.
All your digital notes and treatment plans are linked and cross-referenced within the platform to ensure continuity of care.
You can keep all data in one secure place, or share it with your supervisor and other electronic health record (EHR) systems.
Mentalyc also prioritizes data security and client consent. It doesn't store recordings, and it instantly removes all personal information after sessions. It even gives you the freedom to delete your data whenever you choose.
Plus, the platform complies with HIPAA and SOC 2 security requirements. A signed BAA provides further protection.
Psynth Transforms Your Psychologist Notes Into Accurate, High-Quality Reports
Psynth helps you turn complex clinical notes, test results, and intake data into professional reports in minutes.
Built on validated best practices in psychological reporting and input from expert psychologists, the platform generates high-quality drafts ready for review and finalization.
You can customize the report to your liking while the AI tool automatically handles structure, formatting, and consistency.
Psynth saves valuable hours on report writing. In fact, adopting Psynth has cut reporting time in half for Coast Psychology. As Dr. Morizio puts it, "I spend far less time on tedious tasks like formatting and score transcription, and more time on clinical synthesis."
With Psynth, you can focus on providing better patient care and growing your psychology practice.
Try the platform for free today to transform your reporting workflow!
FAQs About Psychologist Notes
Can I see my psychologist's notes?
Clients can usually access their official records, such as progress notes, but not private process notes. Psychologists may withhold notes that could cause harm or violate mandatory reporting laws. Access depends on clinic policy, documentation type, and legal requirements within your state or country.
What are psychology notes?
Psychology notes are written records of client sessions, including behaviors, progress, and treatment goals. These notes also help psychologists plan care, track improvement, and maintain legal compliance across every stage of therapy.
How to take notes as a psychologist?
Write notes after each session while you can still remember all the details. Focus on client statements, behaviors, and interventions used. Keep the tone professional and factual. Following structured templates like SOAP or DAP helps maintain consistency and meet your ethical responsibility to record accurate, confidential information.
You can also use AI-powered software to automate note-taking and report generation. These tools save valuable time, allowing you to focus on patient care and clinical analysis.
What are some examples of therapy notes?
Popular examples of therapy notes include progress notes summarizing each session, process notes for personal clinical reflections, and intake notes that capture initial assessments. Each one serves a different purpose.



